Introduction
One of my favourite stories that stood out about my maternal grandfather was his decision to get a vasectomy. My mother always narrates the story with a touch of pride as her father had done something that few men did. Reproduction and all its allied issues were and are still considered women’s territory. Men are only present to supply the semen and enjoy sexual pleasure. When my grandfather took it as his responsibility to get a vasectomy, there was a huge uproar at home. For me, the story became synonymous with breaking socio-cultural norms around gender roles, reproduction, and contraception. My grandfather’s action was rational and resulted in a healthier lifestyle. But it also highlights the gendered notion of reproduction and contraception prevalent in society.
Contraceptive methods are seen as a major component to curb population growth. But most often these are addressed to women. A healthy sex life, family planning, and contraceptive methods go hand in hand. But since these taboo topics are not discussed openly, they result in various medical issues, like unwanted pregnancies, STIs, financial instability, health issues for mothers and children, and maternal death.
This paper will explore the taboos surrounding contraception in India where patriarchal norms, mean that the onus of safe sexual intercourse rests only on women. The paper will explore gendered norms, access and acceptance of contraception. A caveat is in order here. Findings of study in different parts of the world suggest that even educated, “middle-class men are unwilling to assume the risks and inconveniences associated with effective contraception, yet expect their female partners to do so” (Laird 1994).
Gendered Norms
The term “women’s problem” encompasses anything pertaining to reproductive health, from periods to pregnancies, to raising children. Contraception is in that sense a “women’s problem”. This understanding is reflected in the way contraception methods are publicised.
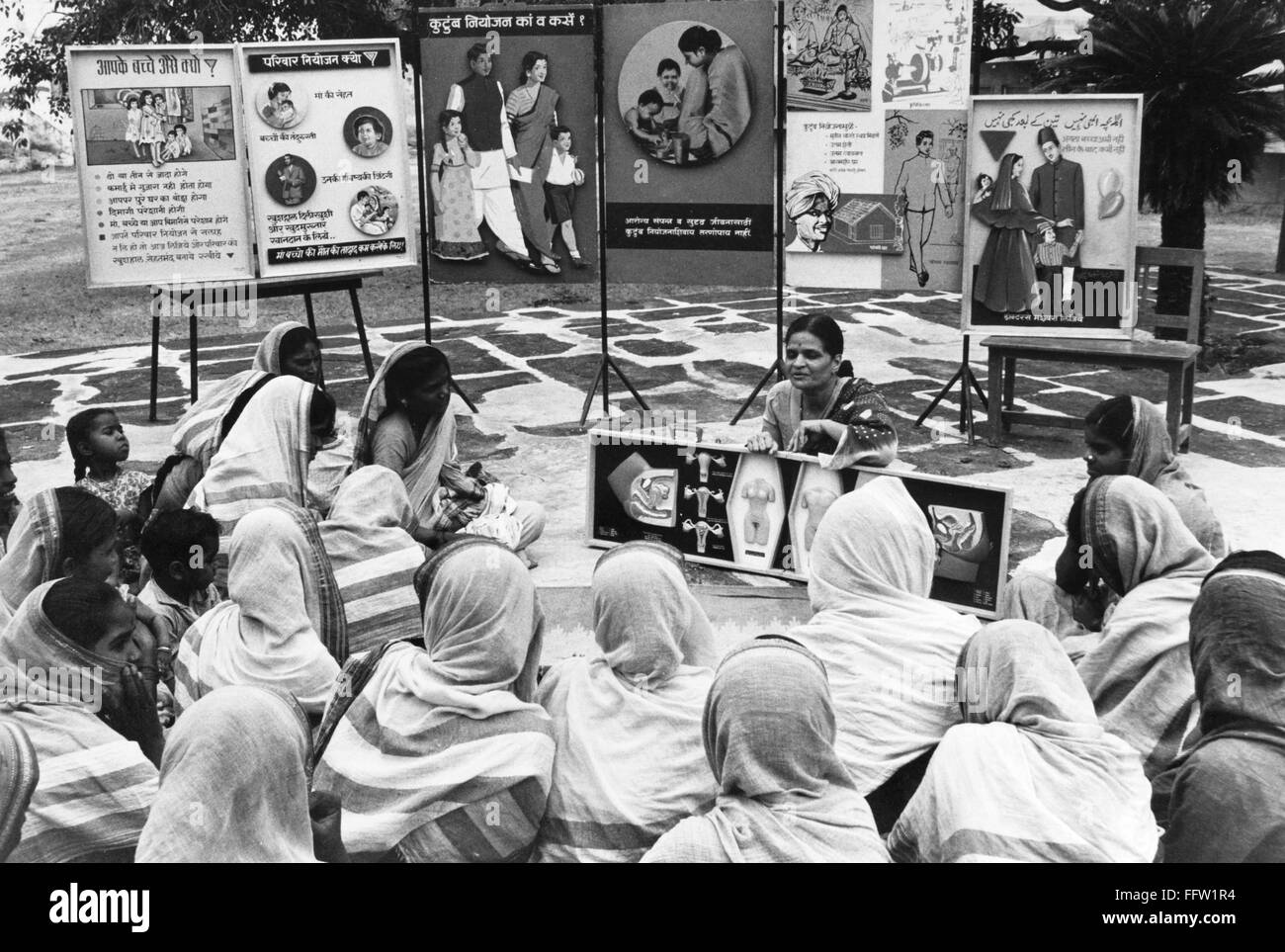
Advertisements on contraceptive products are targeted at women. Most public health workers are women, who interact easily with women in both urban and rural areas. Thus, women are more aware of contraception. Second, men’s source of information on contraception is built around circulating stereotypes. They believe it makes women promiscuous and makes men less masculine. Hence, they don’t want any part of it.
Further, many more female contraceptive methods are easily available. Men are offered only two methods, condoms as temporary and vasectomy as permanent contraceptives. The limited number of male contraceptive methods is often assumed to comprise the major obstacle to greater male responsibility for fertility control. Studies however suggest that the development of more male birth control methods will not be sufficient to increase male involvement in pregnancy prevention given the salience of gender power relationships” (Laird 1994).
Sadhika Tiwari (2020) writes in Scroll.com that though contraception is regarded as women’s responsibility, patriarchal control exists here too. Men are the final decision-makers on using contraception in many households. Many women also agree that men must be the sole decision-makers. According to the National Family Health Survey 2015-16, 75.4% of married men don’t use contraception in India (Tiwari, 2020).
According to the data collected by Family Planning 2020, there is a rise in the usage of contraception since 2012. The data focuses only on women under the categories married and all women. Further, the campaign reflected that the most popular methods used were sterilization of women amounting to 76%, condoms at 11%, and oral contraceptive pills at 8.2%. Sterilization of men only amounts to 0.5%, one of the least used methods.
The huge gap between the top two methods says a lot about the gendered norms practised. This has many adverse implications on women’s lives. This puts them under a lot of pressure to keep up their wifely duties which often jeopardise their health and sex life.
Access and Acceptability
Though the responsibility of contraception falls on women, it isn’t easy for them to access it in society. To access contraception, women’s marital families must be aware of it, especially \husbands. The Ministry of Health and Family Welfare has produced multiple public service advertisements over the years by endorsing contraception like oral pills, Copper-T (IUCD), and condoms to increase awareness. It is interesting to note that most of these advertise female contraceptive methods.
It is also interesting to note that though contraception as a concept is advertised, the social and economic restraints that come with it are ignored. All the ads show the husband, wife, and sometimes even the mother-in-law readily accepting contraceptive methods. But that isn’t the reality for many.
Many women trying to access contraceptives aren’t successful. According to Green (2019), 31 million Indian women don’t have their contraception needs met, the highest in underdeveloped countries. The article talks about two interesting initiatives in Jharkhand, the Saas Bahu Pati Sammelan program and Cyclebeads. These are innovative ideas for safe intercourse. At the same time, they also require open communication and willingness to cooperate between couples, and sometimes even the mother-in-law, which is difficult in India’s patriarchal systems. The article doesn’t specify how successful these programs were.
Contraception and Complications
Women’s contraception isn’t hassle-free as portrayed. They have their problems. Oral pills disrupt the hormonal balance. They have multiple side effects which hinder day-to-day activities, like mood swings, headaches, bloating, and nausea. Hygiene plays a significant role in contraception. IUCD and sterilization must be implemented in a safe and clean environment as they cause infections.
Green (2019) talks about mass sterilization camps at government hospitals causing deaths because doctors perform numerous surgeries in a day, leading to burnout and oversights. But women opt for it because it is cheaper than other methods and easily accessible in rural areas. But the importance of hygiene and post-surgery care isn’t considered and that can cause complications.
Muller and Sengupta (2017) claim that unmet needs for contraception also lead to maternal deaths. According to the article, 45,000 women die from maternal deaths in India every year. Teen pregnancies and malnourished mothers usually lead to maternal deaths. Contraceptives and 3-year gaps between children are emphasised for the mother’s health. Furthermore, regardless of PSAs by the Indian government, access and supply must be constant for this to be implemented.
Access and supply of contraception took a toll during the pandemic. According to Firstpost’s article (2020), contraceptives were not prioritized as essentials and thus many women couldn’t access them. There were reports of a lack of pregnancy tests, where many women weren’t aware of their pregnancies and couldn’t abort on time. Looking at it from a social perspective, a pregnancy, especially an unwanted one, can have life-changing consequences on a mother’s physical, emotional, and mental health as they are responsible for another life, right from conception to childcare and rearing.
Conclusion
The gendered role of contraception on women leads to a lot of issues in their health and society. Contraception is necessary for a healthy lifestyle but the obstacles around it force many to not choose it. The following suggestions can be looked at to tackle this problem. First, contraception must be treated as an open topic by normalizing and bringing more awareness to society. When more people are involved, the responsibility can be shared by people of all genders, especially in decision-making. Second, society might accept it as lifestyle essentials with time and positive awareness. Third, if contraception is demanded publicly, access and affordability can be dealt with. Fourth, with some active government initiative to bring it to the front of healthcare, hygiene and health can be factored in. Fifth, sex education is especially important and must be conveyed as essential and not as taboo as porn. Thus, I argue that when women are burdened with the responsibility of contraception in a patriarchal society, they face multiple disadvantages. This must change, wherein contraception must be considered the responsibility of everyone involved in sexual activities and a part of social life as well.
References:
Family planning. (2020). India-commitment maker since 2012. Accessed on September 20th, 2020. URL Retrieved from: https://www.familyplanning2020.org/india.
Green, Hannah Harris. (2019, February 1). Rural women in India struggle to access contraception. These people are trying to change that. The World. URL Retrieved from: https://theworld.org/stories/2019-02-01/rural-women-india-struggle-access-contraception-these-people-are-trying-change.
Laird J. A male pill? (1994). Gender discrepancies in contraceptive commitment https://pubmed.ncbi.nlm.nih.gov/12346044/
Müller, Ulla and Sengupta, Shumon. (2017, April 11). “In India, Better Access to Contraception Is Key to Reducing Maternal Deaths”. The Wire, Health Section. URL Retrieved from: https://thewire.in/health/india-better-access-contraception-key-reducing-maternal-deaths.
The Associated Press. (2020, August 20). 1.3 million women in India lost access to contraceptives, abortions during the COVID-19 pandemic: report. First Post. URL Retrieved from: https://www.firstpost.com/health/1-3-million-women-in-india-lost-access-to-contraceptives-abortions-during-the-covid-19-pandemic-report-8732021.html.
Tiwari, Sadhika. (2020, September 28). “In India, the burden of contraception still falls on women.” Scroll.com, Family Planning section. URL Retrieved from: https://scroll.in/article/974230/in-india-the-burden-of-contraception-still-falls-on-women.
***
Anaga Sivaramakrishnan is a dutiful bookworm, a writer, and a moody cook. She loves dipping her fingers into different pies to try unique combos. Coming from a mixed socio-cultural background, she claims that this is her way of carving her identity.